Multiple sclerosis overview
Multiple sclerosis (MS) is a neurodegenerative disorder caused by the immune system mistakenly attacking the myelin sheath, a protective coating around nerve fibers. This results in inflammation, which further damages the myelin sheath, as well as the nerve cells themselves and the cells that produce myelin.
What are the types of MS?
There are four types of MS, broadly classified based on disease progression.
Clinically isolated syndrome
Clinically isolated syndrome represents a single event, the first episode of neurological symptoms that typically precedes relapsing forms of MS. On its own, a single event is not enough to define MS, unless patients have evidence of several lesions in their brains. That’s what the “multiple” refers to in “multiple sclerosis.”
Relapsing-remitting multiple sclerosis
Relapsing-remitting multiple sclerosis (RRMS) is the most common type of MS. Patients experience attacks of increasing neurological symptoms, called exacerbations or relapses, followed by periods of partial or complete recovery, called remissions. At various times, patients may have active, not active, or worsening neurological symptoms.
Secondary progressive multiple sclerosis
Secondary progressive multiple sclerosis (SPMS) is the secondary stage of MS that follows RRMS. Patients may have relapsing-remitting episodes initially, but then they experience a steady worsening of neurological symptoms over time that may be accompanied by occasional relapses.
Primary progressive multiple sclerosis
Primary progressive multiple sclerosis (PPMS) affects about 15% of MS patients. Instead of periods of relapses followed by remission, people with PPMS experience a steady decline in neurological function without relapses from the onset of symptoms.
What causes MS?
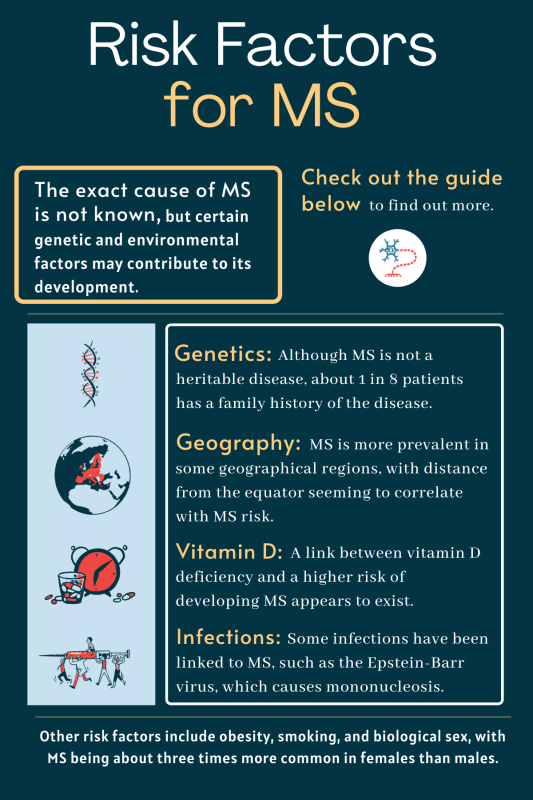
As is the case with many autoimmune diseases, the exact cause of MS is not known.
In autoimmune diseases, the immune system erroneously recognizes the body’s own cells as a foreign threat, and launches an inflammatory attack against them.
Multiple factors likely contribute to the development and progression of MS, and it is believed that both genetic and environmental factors play a role.
Potential risk factors include:
- Genetics: MS is not a heritable disease, although about 1 in 8 patients has a family history of the neurodegenerative disorder. A variant, or mutation, in a gene involved in the immune system, called HLA-DRB1, is thought to be the strongest genetic risk factor for the disease.
- Geography: MS is more prevalent in some geographical regions than others, with the highest disease prevalence found in countries of northern Europe, and throughout the northern U.S., southern Canada, New Zealand, and southern Australia. The distance a person lives from the equator seems to correlate with a risk of developing MS.
- Vitamin D: There appears to be a link between a deficiency of vitamin D, which helps in immune health, and an increased chance of developing MS.
- Smoking: Smoking is linked to an increased risk of developing MS, and evidence suggests that patients who are current or former smokers tend to develop more rapidly progressing forms of the disease.
- Biological sex: MS is about three times as common among females as it is in males. The reason for this difference likely has to do with hormonal and chromosomal differences among the sexes.
- Obesity: People who are obese in childhood and adolescence are at increased risk of MS later in life.
- Infections: Some infections have been linked to MS, particularly the Epstein-Barr virus (EBV), which causes infectious mononucleosis, or mono. A recent study about EBV showed that infection with the virus increases the risk of developing MS by 32 times — the strongest link yet.
What are the symptoms of MS?
MS can cause a wide range of symptoms. These vary from person to person, depending on which specific parts of the nervous system are most affected. Symptom severity also varies widely, meaning that everyone with MS will have a different experience.
Early signs
A concrete list of early signs of MS does not exist, given that disease manifestations can be variable and quite different between affected individuals. A number of symptoms, however, are common to the disease and may be considered early signs of MS.
People concerned they may be experiencing symptoms of the disease are advised to talk with their healthcare provider and keep a record of the occurrence, severity, and duration of their symptoms.
Only a medical professional with specialized training in neurology or nervous system disorders can confirm an MS diagnosis.
Common symptoms
The most common symptoms of the disease include:
- excessive fatigue
- walking difficulties (loss of balance)
- numbness and tingling
- muscle spasms or stiffness
- pain
- vision problems
- bowel or bladder problems
People with MS may also experience emotional changes, including anxiety, depression, and mood swings.
In some patients, the misled immune response causes disease relapses, or periods in which one or more symptoms appear or get substantially worse, followed by periods of partial or complete recovery from symptoms. In others, symptoms steadily worsen over time, with or without the presence of relapses.
How is MS diagnosed?
There is no single test to diagnose MS. Physicians diagnose the disease based on a series of physical and neurological examinations that can help eliminate other conditions.
These tests include magnetic resonance imaging (MRI) that looks for damage in the central nervous system (the brain and spinal cord), and blood and cerebrospinal fluid tests to detect inflammation and specific biomarkers of disease. Evoked potential tests that measure electrical signals from the brain are also frequently used to determine if the speed of electric impulses is impaired.
Is MS treatable?
While no cure currently exists for MS, many treatments are available to help patients manage the disease, and many more experimental therapies for MS are being developed.
Most of these therapies seek to suppress the immune system to reduce inflammation and help protect the myelin sheath; others address specific symptoms of the disease and help patients lead as normal a life as possible.
Because the signs and symptoms of the disease can differ significantly from one patient to another, a team of healthcare professionals usually work together to select the best treatment combination for each person.
Medications currently used to treat MS fall into three main categories:
| Therapy | Purpose |
|---|---|
| Disease-modifying therapies | Prevent relapses and slow the accumulation of disability |
| Relapse management therapies | Shorten the duration and reduce the severity of acute disease exacerbations |
| Symptomatic treatments | Treat specific symptoms of MS, such as pain or fatigue |
What is the prognosis and life expectancy for people with MS?
MS itself is not usually a fatal condition, although it may increase the risk of life-limiting complications, including severe infections. On average, the lifespan for people with MS is about five to 10 years shorter than for the general population, but this gap is closing as treatments and care continue to improve.
Due to therapeutic and healthcare advances, as well as lifestyle adjustments, MS often progresses slowly. Nowadays, about two-thirds of patients retain a fair degree of mobility — the ability to walk, although likely with an assisted device — some 20 years after being diagnosed.
The course of the disease is influenced by each patient’s risk factors, such as having a family member with MS, cigarette smoking, and vitamin D sunlight exposure. MS prognosis is generally better for people with relapsing-remitting MS than for those with progressive forms of MS.
What other conditions could MS be mistaken for?
As a neurodegenerative and autoimmune disease, MS may share some symptoms and signs with other conditions — especially in the early stages — which may lead to misdiagnosis.
ALS
Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, is a progressive neurological disorder that damages nerve cells and causes disability, as MS does. The exact causes of MS and ALS are not clearly understood, but genetic, environmental, and lifestyle factors are believed to play a role in both diseases.
ALS, however, particularly affects motor neurons, the nerve cells that control voluntary movements. Within a few years of diagnosis, ALS patients usually lose the ability to perform everyday tasks including walking up steps, reaching for items, or dressing themselves.
MS can also have a significant impact on a patient’s mobility and physical capacity both MS and ALS are characterized by fatigue, muscle stiffness and spasms that interfere with movement — but, as it often happens in the latter stages of ALS, only in some cases does MS leave a person completely debilitated and/or paralyzed.
Some ALS patients may reach a state called locked-in syndrome, where their mind is fully intact, but they have lost voluntary control over their body’s movements. In contrast, MS can affect a person’s cognition and cause difficulty with thinking, learning, and problem-solving.
Parkinson’s disease
Parkinson’s disease (PD) is a neurodegenerative condition that affects the brain, resulting in a progressive loss of coordination and in movement problems. As in MS, the exact causes of Parkinson’s are not yet clear, but environmental and genetic factors are thought to play a role.
The disease is characterized by the death and dysfunction of nerve cells, especially dopaminergic neurons — nerve cells that communicate with other neurons by releasing a signaling molecule called dopamine.
Parkinson’s disease can cause motor symptoms such as tremor, abnormally slow movements (bradykinesia), and muscle rigidity. Problems with balance and walking are also common. The disease also can cause non-motor symptoms such as cognitive impairment, depression, sleep problems, and hallucinations or delusions.
Parkinson’s is usually diagnosed in those ages 60 or older, although it can also affect younger adults. MS usually affects people around the ages of 20 to 50, as well as children.
Myasthenia gravis
Myasthenia gravis (MG) is a neuromuscular condition triggered by an autoimmune response. The specific cause of MG is unknown, although evidence suggests that the thymus gland — which is part of the immune system — may help trigger or sustain the production of harmful autoantibodies that disrupt the normal communication between nerve cells and muscles.
MG causes muscle weakness and localized fatigue in certain muscles. Usually, the first signs of the disease are drooping eyelids and double vision. In some patients, difficulty swallowing and talking are the first disease manifestations.
Double vision, difficulty with walking, speaking, chewing, and/or swallowing are symptoms shared by MG and MS.
Although MG can occur at any age, it most commonly manifests in women when they are in their 20s or 30s and in men when they are in their 50s or 60s.
| Disease | Symptoms | Diagnosis | Progression |
|---|---|---|---|
| MS | Abnormal sensations, spasticity, bladder and bowel complications, vision problems | Most commonly diagnosed in people ages 20 to 50 | Can have significant impact on many facets of life but does not leave patients completely debilitated |
| ALS | Muscle weakness, twitches, pain, breathing difficulties, dysphagia, speech problems | Symptoms typically begin around ages 55 to 75 | Symptoms worsen over time, leading to complete debilitation and paralysis |
| PD | Resting tremor, slowness of movement, muscle stiffness, fatigue, cognitive changes | Generally begins later in life, with most cases beginning around age 60 | Is not fatal but can put substantial strain on the body and make people more vulnerable to infections |
| MG | Droopy eyelids, blurred vision, slurred speech, weakness in the arms and legs | Most commonly affects women under the age of 40 and men over the age of 60 | Symptoms may come and go but generally worsen over time |
What are some other diseases related to MS?
Besides MS, several other neurological conditions are also caused by an inflammatory attack that damages the myelin sheath. These are collectively called demyelinating diseases, and include:
- transverse myelitis
- acute disseminated encephalomyelitis
- neuromyelitis optica spectrum disorder
The location and number of lesions on MRI scans, as well as the resulting symptoms, are among the factors that help distinguish between MS and these related demyelinating disorders.
Transverse myelitis
In transverse myelitis, the inflammation and myelin damage are found in the spinal cord. Classic symptoms include weakness in the limbs, abnormal sensations (numbness or tingling), pain and discomfort, and bladder and bowel issues.
While transverse myelitis can occur on its own, often after a viral or bacterial infection, the condition can also be associated with multiple sclerosis. In fact, transverse myelitis can not only present as a first symptom of MS, but people with transverse myelitis who present with more than two lesions seem to be much more likely to develop MS.
Most people affected by transverse myelitis have at least partial recovery — most recover within the first three months after the attack. Others may experience permanent impairments that affect their daily living. Some patients will only experience one episode of transverse myelitis, while others may have a recurrence, especially if an underlying medical condition caused the disorder.
Acute disseminated encephalomyelitis
Acute disseminated encephalomyelitis, or ADEM, usually consists of a single event or attack that causes myelin damage. The brain, spinal cord, and occasionally the optic nerve can be affected in ADEM patients.
As with MS, ADEM is characterized by symptoms such as visual impairment, weakness, numbness, and loss of coordination and balance. In contrast, fever, seizures, confusion, headache, nausea, and vomiting are common ADEM signs but are not usually seen in MS patients. Also different from MS, people with ADEM may experience some degree of impairment of consciousness, even coma.
The exact cause of ADEM is not clear, but in most cases, the disease is thought to be triggered by a response to a viral or bacterial infection. Very rarely, ADEM can follow a vaccination.
Unlike MS, children are more likely to develop ADEM than adults. The disease is also more common in males, which highly contrasts with MS.
Physicians usually carefully monitor people with ADEM or transverse myelitis to see if a recurrence suggests MS.
Neuromyelitis optica spectrum disorder
Neuromyelitis optica spectrum disorder (NMOSD) is a progressive autoimmune disease that affects the nervous system. It primarily leads to inflammation of the optic nerve — the nerve that sends and receives signals from the eye — and the spinal cord. This leads to issues with vision and the control of muscles.
The disease is characterized by pain inside the eye, blurry vision, and potential vision loss when the optic nerve is affected. When the spinal cord is affected, symptoms include weakness or paralysis of the limbs, loss of sensation, pain, muscle spasticity, trouble breathing, and inability to control the bladder and bowel.
Although NMOSD primarily affects the optic nerves and the spinal cord, it can also attack the brain and, as in MS, the disease can lead to psychological issues, including depression and impaired cognition (thinking).
As with many autoimmune diseases, the exact cause of autoimmunity in NMOSD is not clear, but both genetic and environmental factors are thought to play a role.
NMOSD is considered a relapsing-remitting disease, characterized by periods of relapse and remission, similar to some forms of MS. Unlike MS, however, there is no progressive phase of this disease. Symptoms are generally more severe after an NMO attack compared with an MS attack.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
FAQs about multiple sclerosis
A condition called clinically isolated syndrome (CIS) is considered the first clinical presentation of disease. People with CIS may never experience another episode of symptoms, or they could progress to full MS. Most people with MS (about 85%) are diagnosed with relapsing-remitting MS, which is characterized by disease relapses and periods of remission. About 10–15% of patients are diagnosed with primary progressive MS at disease onset — an MS type in which symptoms steadily worsen over time.
MS is not considered a hereditary disease; however, about 1 in 8 patients have a family history of MS, suggesting a genetic component that may contribute to the development of the disease. It is estimated that about 200 genes may, to some extent, play a role in MS development.
MS is characterized by the body’s immune system attack to the central nervous system — the brain, spinal cord, and optic nerves. Symptoms vary depending on which specific parts are most affected. Problems with vision and movement, as well as numbness or tingling sensations, are often reported by patients.
MS is a chronic, lifelong disease, and symptoms generally get worse over time, potentially causing physical disability, cognitive difficulties, and emotional challenges. Walking can become difficult, and many patients eventually need an assistive device such as a cane, walker, or wheelchair. MS can decrease a person’s quality of life by interfering with one’s ability to work and to carry on usual life activities.
MS itself is rarely fatal but, depending on the severity of the disease, it may increase the risk of life-limiting complications including severe infections and swallowing difficulties.
 Fact-checked by
Fact-checked by