Need to Know: Do I Need Contrast Dye for an MRI?
Editor’s note: “Need to Know” is a series inspired by common forum questions and comments from readers. Have a comment or question about MS? Visit our forum. This week’s question is inspired by the forum topic “Gadolinium – The contrast agent used in MRI scans,” from April 10, 2018.
MRI: A brief history
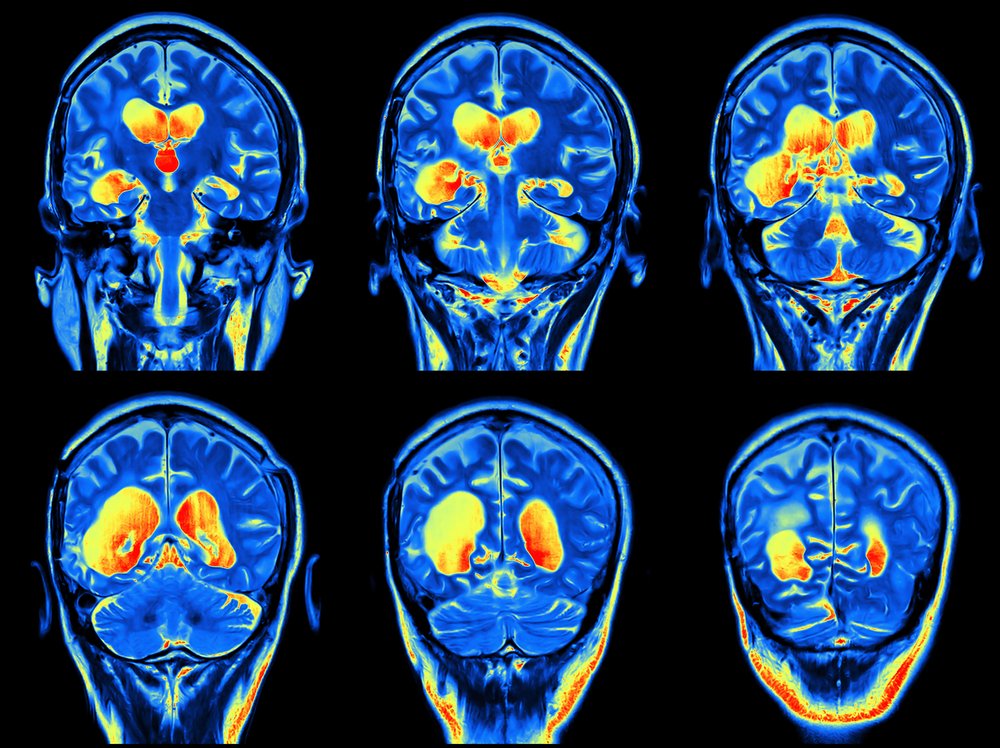
Magnetic resonance imaging (MRI) uses magnets to measure molecular activity in the soft tissues of the body, including the brain. Because it’s a noninvasive way to “take a picture” of your insides, it’s become the go-to diagnostic and assessment tool for identifying and measuring MS disease activity.
The first MRI test on a human being took place in 1977 for cancer research. Four years later, the technology was used to scan the brain of a person with MS, generating the first images of lesion activity. In 1988, the first contrast dye, a gadolinium-based contrast agent (GBCA) known as gadopentetate dimeglumine, was used to enhance MRI scans for better interpretation.
Since then, MRIs with and without contrast have been a mainstay of disease management for decades.
What is gadolinium dye?
Gadolinium is a rare earth mineral (Gd, No. 64 on the Periodic Table of Elements). It is bonded, then converted to a dye medium. In this state, it’s injected into a vein during MRI scanning to provide imaging contrast. This contrast allows a specialist to best interpret MS disease activity.
The dye, in early research, was thought to be eliminated as a waste product by the kidneys. However, more recent research suggests that about 1 percent of an injected dose of gadolinium dye may be retained in the tissues and bones.
The problem with gadolinium dye
Dye retention
Controversy over GBCAs has centered on these deposits. Science does not have a clear understanding of the risks these deposits may pose in the long term.
A rare condition known as nephrogenic systemic fibrosis, which occurs in patients with preexisting kidney failure, is the only known adverse health effect related to gadolinium retention.
However, reports of adverse events “involving multiple organ systems in patients with normal kidney function” have also been reported, though no link to gadolinium retention has been established.
The U.S. Food and Drug Administration issued new warnings in January 2018 regarding the use of GBCAs in tandem with MRI after reviewing safety concerns.
Adverse reactions
There is no easy way to predict who will have a negative reaction to gadolinium dye, but unfortunately, some people do not tolerate it well.
Most commonly, side effects include brief dizziness, nausea, and headache. However, about 1 in 1,000 patients may experience an itchy injection site rash.
The most severe reaction — anaphylaxis (difficulty breathing and swelling of the throat and lips) — occurs at a rate of about 1 in 10,000.
Research update: Gadolinium dye
Research published in the journal Radiology last March, titled “Accuracy of Unenhanced MRI in the Detection of New Brain Lesions in Multiple Sclerosis,” suggests that the use of contrast dye to enhance MRI scan images may no longer be necessary.
The retrospective study evaluated over 500 follow-up MRI images from 359 MS patients using a variety of methods for comparison. Based on the study’s findings, the study’s co-authors wrote: “In none of the 507 images did the contrast-enhanced sequences reveal interval progression that was missed in the readouts of the nonenhanced sequences. …”
Researchers concluded that scans that employ a 3T MRI* (a higher powered scanner used in research), when used in combination with new artificial intelligence techniques, are “ready to supersede routine use of contrast material in most instances of follow-up investigations of patients with MS, reducing both imaging time and cost without missing new or enlarged lesions.”
The Radiological Society of North America announced the findings in a press release.
***
*Patient and clinical access to a 3T MRI scanner can vary widely.
Do you have a story about contrast dye you want to share? What questions do you still have about GBCAs? Post your replies in the comments below or at the original “Gadolinium – The contrast agent used in MRI scans” forum entry.
***
Note: Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Multiple Sclerosis News Today or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to multiple sclerosis.







Bill.
My doctors keep all the MRIs to track disease progression. They have AI to monitor brian atrophy. Unless new symptoms or annual MRI show something new they do not use contrast. So for me have not used in 7 years since the first attack. N
Tamara Sellman
That's the case for me, too, Bill (at least now it is).
Tamara
Judy Crutchfield
Are MRI’s needed after you have been diagnosed? My doctor does not do them because he says right now there is no cure so what good would it do. Should I find a new doctor?
Karen
Judy - An MRI can tell part of the story of your disease course, and help inform treatment options. please reaserch HSCT. It has an 80% success rate of stopping disease progression.
Tamara Sellman
If you're stable, then you can go a while without having them. I'm on the 2-year schedule now (I graduated! LOL) and will only have one if I have new symptoms or extreme versions of my old symptoms that last more than a couple of days. But for a doctor to say "there is no cure so what good would it do" seems very concerning to me. If you have mild MS and slow progression, then maybe... but for people with more active disease, MRIs are the only way to track it, and you don't always know you have active disease. My two cents, anyway. If you feel like your MD is dismissive, maybe you should consider looking for a new neuro?
Tamara
Janice B.
Thank you for this article. I have had RRMS for 37 years. I have yearly check ups with my Neurologist and have refused yearly MRIs with and without GBCAs since 2010 as my symptoms have remained stable. In 2015 I was diagnosed with Smoldering Myeloma which remains stable based on regular check ups with my Oncology Hematologist. There is research published online suggesting a potential link between having an MRI with GBCA and the acceleration of Smoldering Myeloma to Stage One Myeloma. My Neurologist stated that having an MRI without contrast would reveal any new lesions but would not show changes or activity in existing lesions (if there are any). I’m unsure about having an MRI with contrast in the future should the need arise as I wouldn’t want to cause my Smoldering Myeloma advance to Stage One Myeloma . Any input or personal experience someone might share is most appreciated!
Tamara Sellman
Hi Janice
you're welcome :)
I cannot add much to your inquiries about Smoldering Myeloma (except that I wonder why they have to give it such a scary name??) It seems to me that more information is better information, at least for me, so it comes down to risk-benefit analysis... is the MRI with contrast worth the information it delivers within the context of your myeloma concerns? Only you can decide that, but maybe there are others in this community who could share their experiences. I hope you can keep that SM under wraps and wish you well moving forward!
Tamara
susan k irwin
Chuck Norris's wife became deathly sick from contrast with MRI. Gadolium went to the deep tissues of her body that she said felt like acid. She had to go abroad to get help detoxifying from it. Doctors would not acknowlede it was the contrast that did it. I wont take contrast.
Melanie
Hi. I feel the same way about contrast. Can you refuse it ? Can they still get good images without it.
MONICA
It would be worth it to drive to a 3t machine. We have one in my town.
Chris
Hi
What town do you live in that has a t3 machine?
I do not want the contrast even though my dr has requested with and without.
I just came out of years of mild kidney failure and have autoimmune issues. Now we think I may have MS…and MRI is ordered.
Thanks.
Alan S
I've been declining contrast for years against doctor's orders. Since contrast only allows the doctor you see if there is any current inflammation, I never understood the point if I wasn't having an exacerbation. If there were any new lesions, whether 2 weeks or 2 months old, they would still show on a normal MRI. And if I were in an exacerbation, I'd know it anyway.
Joanne Perkins
I will not ever have a MRI using gadolinium contrast again. I had a concomitant symptom of a swollen left kidney and urinary difficulty after receiving it. This symptom has not subsided since 2016.
Tamara Sellman
I'm sorry to hear this, Joanne. I do wonder how many people have experienced unnecessary damage to organs because of this dye. I hope you find relief!
Tamara
Jan Charles
I was participating in an MS study about 20 years ago. Each month I would be infused with Omniscan with no problems. For my last scan, within seconds of the dye being infused, I knew something was wrong. I felt a fire going through my vein and into my chest. I had trouble breathing within 30 seconds. IV Benadryl turned me around before my throat closed up. What had happened was that they had used a different agent, Magnavist. From that time forward I have been able to obtain Omniscan for subsequent scans. I wonder why only one agent is easily available now.
Tamara Sellman
Thank you for sharing this insight, Jan, and what an ordeal you must have had! Who knows why these agents are picked, one over the other, in the first place? I'm glad you were able to get through the allergic reaction with the Magnavist, that must have been awful.
Tamara
tracy a williams
I was told that you can not consent to the contrast and that your doctor is supposed to tell you that before the procedure and obtain your signature.
Tamara Sellman
That sounds right to me, Tracy. I think a lot of doctors are going this route, or not using it at all, but it's good for us patients to know we have the option to say no.
Tamara
Jana
I was diagnosed with RRMS 2007 and have been receiving Gandolinium for my MRI’s. I had a very severe case that nearly killed me. During the 2 months of severe deterioration, I was scanned, what seemed like, twice a week. At the beginning, the contrast didn’t affect me at all. Once I was discharged, I got scanned every six months until I started feeling a little funny right after receiving the Gandolinium. I shrugged it off. A year later, I had another MRI with prednisone and Benadryl to help with the allergic symptoms. I felt worse. I again didn’t think much of it because it lasted about 5 minutes. I spoke with my neurologist regarding my symptoms after receiving the contrast and how the symptoms had progressively gotten slightly worse. She again wanted another MRI a year later and I simply didn’t comply because I had been recovering and doing better. I repeated the MRI with contrast two years later. This time it really scared me and I did not accept having another MRI with contrast again. My neurologist now says that it isn’t necessary because I’ve been doing well. I wonder if I had never said anything, I could have been adding more unnecessary possibly harmful minerals to my body. I still hope that it doesn’t affect me in the future.
The symptoms I felt with the contrast were dizziness and I felt the contrast go up from my stomach to my throat. It felt as if my airway was blocked. It was pretty scary. I told my neurologist that I must be allergic to contrast. I also felt as if no one believed me. I’m glad people are becoming aware of this!
Tamara Sellman
Thank you for sharing this experience with us, Jana. When people read this, they'll be more knowledgeable of the risks and perhaps more empowered to speak out against these risk factors. It's hard to advocate for oneself but totally worth it, as your example shows.
Tamara
Emm
I'm scheduled for an MRI w/wo contrast in a few weeks. My neurologist says I have CIS, so naturally a round of tests have been ordered.
If anyone can help: Does the first MRI absolutely need imaging with contrast? I suppose if it's the only way to get a definitive answer, I'll consent, but otherwise I'd really like to forego this. I don't have kidney failure, but my kidneys aren't in the best of shape as I've had multiple kidney infections over the years.
Also, what a great website! I've been browsing around the last couple days since I'm new to the CIS/MS "club" and am trying to learn as much as possible.
Tamara Sellman
Thanks for writing, Emm. It's a tricky question, one that might be best answered by your neurologist. Contrast might be used initially to get an accurate baseline image of your lesions to reference against in the future. If you're concerned about kidney damage, share that with your doctor. It may depend on the quality and type of imaging equipment they have available to them. Good luck!
Tamara
Summer Victoria Guilmette
I am getting an MRI at the end of May and I am really nervous. Can I say no to the iv? I hate needles in general.
Any advice that you guys can give me would be awesome at this point in time would be awesome.
Amanda
How did the MRI go? did you decline the injection?
M
when you are having your first MRI in order to diagnose or rule out MS is it necessary to use contrast to identify the lesions? I had my MRI with and without but the report I received was for without and showed no lesions. Did they not send me the MRI results with contrast as they would not be any different? Thx!
Tamara Sellman
I think it depends upon each patient and their specialist. If you want to know your results and feel you didn't receive them all, you should be able to ask your specialist to go over all of them with you. You have a right to access all of your records and to receive a full report on their findings. If you have a private patient account where you can log in online, you might be able to see them posted there. Good luck!
Tamara
Betty Hayes
I had an MRI with Gadolinium contrast in my brain six years ago. When the contrast went into my system I felt it go to my brain and I felt my blood pressure bottom out! The operator had said it would only be about five minutes more so I wanted to try to hang on rather than have to do it all again. The operator came to the machine and when I came out she told me it was over and that I could sit up. I tried to sit up and passed out! They brought me to an I was on a stretcher in an outer hallway. I was clams and my blood pressure was 70 over 47. When they tried to sit me up again I passed out again.
I was worried about my dogs, some of which were ill and I wanted to go home, but they said I could not. A man in the hallway kept saying they needed to get me to the hospital on the same campus but the nurse kept insisting that she was handling it and that I would be ok. I felt weak, scared and disoriented! They kept me in that hallway for about two hours and would not let me leave.
When I picked up a copy of the medical records the report was not factual! The blood pressure readings were changed and the report only said that I was near whatever the word for fainting was!
I now am informing all of my doctors of this episode and when I tell them they nearly freak out! I list it as an allergic reaction, but it was severe! And I don’t know if that is the reason for some of my conditions that I now have to suffer!
Tamara Sellman
That's a terrible thing to go through, Betty. <3 Tamara
Shelley
Hi, I’ve been having some odd sensory problems with my legs and arms. The neurologist sent me for an mri to see if there was any inflammation but none was spotted. I’ve now been asked to have an mri with dye. Would this be necessary to rule out ms? Would early me show on an mri without contrast? If anyone has any experience or knowledge on this I would be very grateful.
Tamara Sellman
Dyes can provide a clearer picture and make inflammation easier to spot. These days, there's a lot of concern about using dye, but doctors may still need to use it in order to get the best possible information from your MRI. My sense is that you should ask your doctor if it's absolutely necessary... and if it is, then this is probably why. Good luck!
Tamara
S Sandeman
Thank you for your reply. I've had my mri and am still waiting for the results. The dye was not a problem for me. It's been a long wait because of Christmas and new year. I'm told it will still be another week or so before I get any results. I'm hopeful as nothing showed up on my first mri it is nothing serious and I'm guessing it's unlikely to be MS because of that? I guess I'll have to wait and see!
happy New Year to you all, Shelley
Tamara Sellman
Glad you were able to tolerate the dye! Do keep us posted on what you find out! The whole diagnostic journey is such a mysterious one.
Tamara
Danny
This is my second time having a kidney stone when the did the scan it showed me having two spots on my kidney the top
And bottom also the kidney stone I did have the dye injected in be before a few years back I do have to get a another scan in a week with the dye injected in me so they can see what the two spots are the doctor said I had nothing to worry about do you think from other people here experiences should I go with this procedure
Tamara Sellman
I would say that, if the doctor says you have nothing to worry about, and you trust them, then I wouldn't worry. They do have new dyes that aren't gadolinium that can still achieve what they need during MRI. Best wishes,
Tamara
CAWS
And what would those new dyes be? I have not been able to access the new Mn based dye for MRI in USA as it is not approved even though non toxic. I have been told my only option for MRI dye is Gadolinium which I cannot & will not take.
ANNE-MARIE
Hello,
My first scan I was given the dye but since then I have not been given it. I see my neurologist last year and he said my lesions in my spine and brain were not active. How can they tell if you have not had the dye???? I have SPMS and at the moment confused after reading that you need the dye for them to see if your lesions are active.
Tamara Sellman
Hi Anne-Marie
Have you tried just asking your neurologist? It might be that they already have enough information from your current scans and don't feel the need to use the dye. It really depends upon the type of machine they use, your particular disease course, where your activity is, and a lot of other variables. It would be best to approach your doctor with this question, they should be happy to explain why they omit the dye. For what it's worth, my neuro doesn't always use the dye anymore, either. I've been in remission since 2014, so that might be part of it. Good luck, Tamara
Melissa Bougie
I have a question. I had done an MRI on January 2020 and they seen ms in my neck/spinal cord and they used the dye, I just had another MRI done Feb 26th 2020 and apparently they didn't see anything. What do you suggest? Should they do another MRI with the dye?
Tamara Sellman
Hi Melissa
It's hard to say. Maybe they said they didn't see anything NEW. If you've been given an MS diagnosis, then those lesions on your neck/spinal cord will always be detectable on MRI, but they will be observed as active or inactive. If they said they didn't see anything, then they might have meant they didn't see anything concerning or new. But I have no idea, as I'm not a doctor, so you'd be better off asking your doctor this question directly. They should take the time to explain what they meant by that. Good luck to you!
Tamara
Schubert
I'm seeing a colorectal surgery doctor on February 24(Wednesday). I did a colonoscopy last September 21st, negative finding. but my left side abdomen still in pain from time to time. so I might be asked to go MRI or CT? Compare these two scans, first I would exclude CT because of its high dose of radiation plus contrast agent, double harms to our bodies. That left only one choice -- MRI. I am wondering. Is it possible to go MRI without a contrast agent for my abdomen scan? Do we have to do MRI with a contrast agent? I don't know what to do. So afraid of the contrast. Since it will be left in my body entire life according to FDA 2018 communication. and only Dotarem, Gadavist and ProHance are Macrocyclic agents which remaining in the body are LOWEST after use of these. What if this hospital doesn't have one of these three brands? Can I say no to the doctor?
Ruth
I have just had an MRI, my Neurologist requested contrast, as the scan was being done the images were being reviewed by a doctor (i have never known this before and this is my 8th scan) the Doctor decided i did not require the contrast injection i am now confused as to why that decision was made? I did not get to see said Doctor as i was in the machine.
Pam Williams
Is it necessary to have a cardiac MRI with contrast to check a left bundle branch block. The cardiologist already did a heart cath 3 weeks ago. All the arteries were clear. I'm very hesitant to have the contrast. I have been detoxing since I had the heart cath which uses lot of radiation and dye. The gadolinium contrast doesn't sound safe to me.