FAQs about secondary progressive MS
No form of multiple sclerosis (MS) is itself fatal, though the disease may increase the risk of life-threatening complications such as pneumonia or trouble swallowing. The average life expectancy for someone with MS is around five to 10 years less than the general population, though this gap is continuing to narrow as care for multiple sclerosis patients gets better and better.
Secondary progressive multiple sclerosis (SPMS) is characterized by symptoms that gradually get worse over time. Specific symptoms and rates of progression vary widely from person to person, but it is common for SPMS symptoms to cause challenges in day-to-day life, making certain activities difficult or impossible to do independently. Most people with SPMS will retain some ability to walk, though many rely on aids such as a cane, walker, or wheelchair to help them get around.
For most of human history, nearly all people with relapsing-remitting multiple sclerosis (RRMS) have eventually developed secondary progressive multiple sclerosis (SPMS). However, modern treatments can delay this transition, and it is becoming more and more common for people to live with RRMS for decades without transitioning to SPMS. Nowadays, some people with RRMS will go their entire lives without developing SPMS.
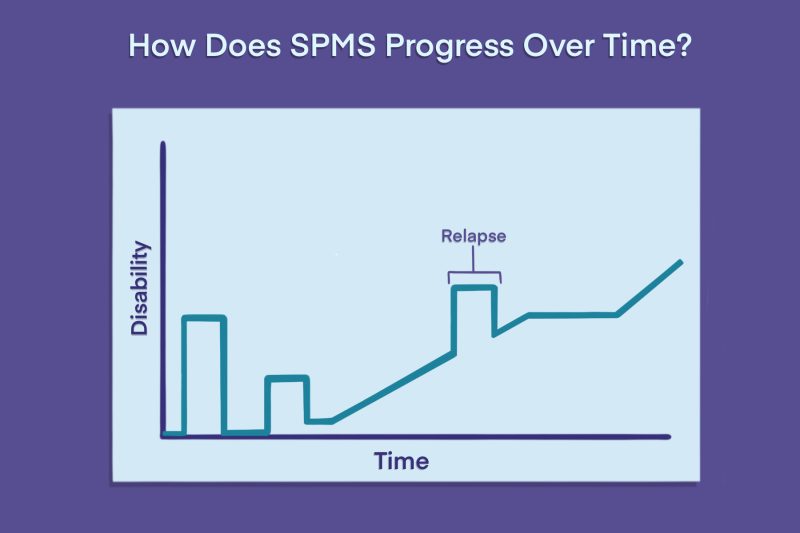
Relapsing-remitting multiple sclerosis (RRMS) is marked by bouts of suddenly worsening symptoms, called relapses, interspersed with periods of remission where symptoms ease or vanish entirely. Secondary progressive multiple sclerosis (SPMS) develops after RRMS, and is marked by continuously worsening symptoms independent of relapse activity. As such, symptoms are generally more severe in the SPMS stage than in the RRMS stage, and disabling symptoms tend to accumulate more quickly in SPMS.
Secondary progressive multiple sclerosis (SPMS) can cause symptoms like muscle spasticity, fatigue, and coordination problems that may make walking difficult. Some patients rely on a wheelchair to help them get around. More than two-thirds of SPMS patients retain some ability to walk, though some may need an aid like a cane or walker to do so, and others may also use wheelchairs at times to help be more active and save energy.
Related Articles

 Fact-checked by
Fact-checked by