Switching strategies: When to change your MS therapy
Last updated Jan. 15, 2025, by Marisa Wexler, MS

It’s generally recommended people with multiple sclerosis (MS) start treatment as early as possible after their diagnosis. However, there are a range of different MS treatments, each with its own safety and efficacy profile, and it’s not uncommon to need to switch MS treatments.
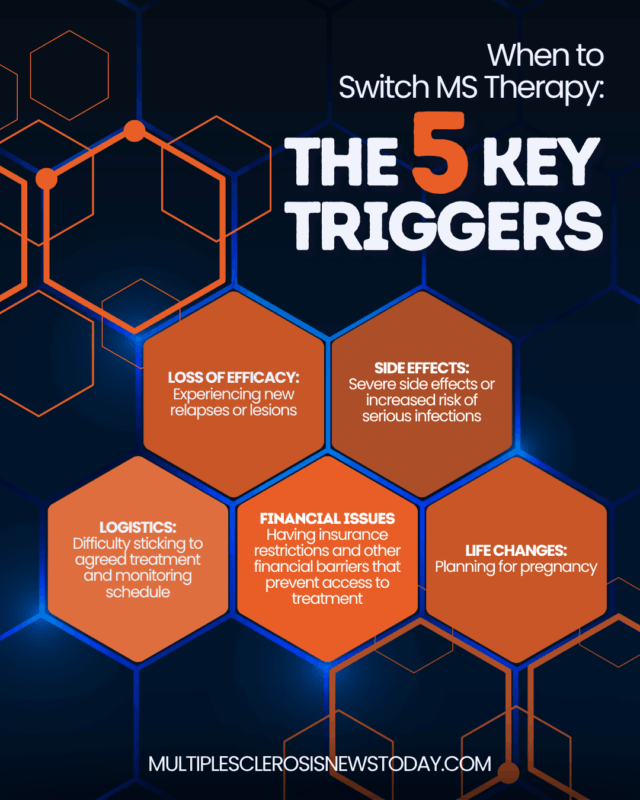
At some point, your treatment may no longer be adequately managing your MS or may be causing debilitating side effects. Perhaps logistical or financial constraints are the reason for making a change, or maybe you are thinking about getting pregnant.
The decision of whether to switch treatments — and which specific therapy to switch to — should always be made in close collaboration with your care team. They will consider a number of factors, such as your disease type and how active it is, and will also weigh the potential benefits and risks of each therapy for your specific situation.
How your MS type affects treatment
MS can be broadly divided into four main types:
- Clinically isolated syndrome (CIS) is the first event of MS-like symptoms. While not technically MS, it may progress to clinically definite MS in some people.
- Relapsing-remitting MS (RRMS) accounts for about 85% of all newly diagnosed patients. RRMS is characterized by relapses, where symptoms suddenly worsen, followed by remissions where symptoms ease or disappear entirely.
- Secondary progressive MS (SPMS) is a disease stage that follows RRMS. It’s marked by the gradual worsening of symptoms, even when the person does not experience any relapses.
- Primary progressive MS (PPMS) accounts for about 15% of newly diagnosed cases. At onset, symptoms gradually worsen without periods of relapse and remission.
The vast majority of MS disease-modifying therapies (DMTs) are approved for relapsing forms of MS, including CIS, RRMS, and active SPMS, which is when there are still occasional relapses or evidence of disease activity in MRI scans.
Relapsing forms of MS have been easier to treat, so you and your doctor have a lot of options to choose from. There are far fewer treatments proven effective for nonactive SPMS and PPMS, so options for progressive MS management are much more limited.
Current therapies for MS
In the U.S., nearly two dozen different treatments are available for relapsing types of MS. Different medications work through slightly different mechanisms, but in general, all of the available treatments aim to reduce the activity of the immune system to dampen the inflammation that drives MS.
Because they block inflammation, DMTs can help reduce the frequency and severity of disease relapses, prevent new or enlarging lesions, and/or slow the accumulation of disability. However, these drugs generally cannot repair existing damage, so they are unable to reverse symptoms you already have.
For this reason, people with MS should start treatment with a DMT as early as possible — before the disease causes irreversible damage to the brain and spinal cord — which can improve long-term outcomes.
There are many treatment classes approved for MS, each with its own mechanism of action, efficacy, route and frequency of administration, and common side effects. Even within the same class, there may be differences between each drug, which should always be considered when deciding which treatment is best for you.
It is often recommended after being diagnosed with MS that you start treatment with a highly effective DMT, such as a CD20 inhibitor or another antibody-based therapy. While these newer medications may have a higher risk of serious side effects compared with older, moderately effective therapies, their greater potency can help delay the progression of disability, giving you a better chance to maintain your abilities and quality of life for longer.
Because MS varies greatly in every person there isn’t one DMT that’s best for everyone. For instance, your doctors may recommend starting with a moderate-efficacy therapy if your MS is stable or if you have a higher risk of side effects. If needed, they can adjust your treatment plan over time, potentially switching to a more effective therapy as your situation evolves.
When deciding which DMT to use, your healthcare team will work closely with you to find the right balance of effectiveness and safety.
Symptom progression
The two main mechanisms involved in MS symptom progression and increasing a person’s disability level over time are relapse-associated worsening (RAW) and progression independent of relapse activity (PIRA).
RAW occurs when you experience a relapse or flare-up of symptoms and have an incomplete recovery, meaning some symptoms that appeared or worsened during the relapse did not completely disappear after the relapse ended.
PIRA refers to the gradual worsening of disability that occurs unrelated to relapses. It reflects the “silent” accumulation of nerve damage from chronic inflammation and other disease processes, even when the inflammatory activity responsible for relapses is well controlled.
While RRMS progression was believed to be mainly driven by RAW, recent research shows PIRA is the main contributor to disability progression across all disease types.
Because approved DMTs can reduce the risk of relapses, they are very effective at preventing RAW. There’s also evidence some existing therapies can help reduce the long-term risk of PIRA, but more effective treatments are needed to better address this type of progression.
Limitations with DMTs
While available MS therapy options have been proven in clinical trials to reduce the frequency of relapses, decrease lesion burden, and slow the accumulation of disability over time, they have limitations that may prompt changing MS medication at any point in the disease course.
These limitations may include:
- lack or loss of efficacy, particularly as your MS progresses
- increased susceptibility to infections, including serious opportunistic infections
- unmanageable or debilitating side effects and infusion reactions
- challenges with frequent disease monitoring required for certain medications
- insurance restrictions and financial barriers to accessing treatments
- inconvenient treatment schedules or modes of administration
- changes in personal circumstances that affect adherence or treatment preferences.
Regardless of where you are in your disease course, either newly diagnosed or living with MS for several decades, finding the right DMT will always require you and your doctor weigh potential side effects against the potential benefits of any medication. Logistical factors related to treatments, such as access, cost, and how it is administered, should also be considered.
When to consider switching your MS therapy
While DMTs play a vital role in managing MS, individual needs and circumstances can change over time. Switching therapies is a common part of MS management and may be considered for several reasons.
Lack of efficacy
While some therapies are more effective than others, none is 100% effective at controlling MS. For this reason, it’s not uncommon for someone with RRMS to experience breakthrough disease activity while receiving an approved DMT. If this happens, you may want to consider switching medications.
Guidelines from the American Academy of Neurology recommend trying another DMT with a different mechanism of action or with higher potency if you:
- experience at least one new disease relapse
- have at least two new lesions visible on MRI scans
- experience continual worsening of disability for at least one year.
DMTs usually take some time (typically a few months) to become fully effective. It’s possible to have new signs of disease activity in the first few months after starting on a new medication. Your neurologist will generally wait until the DMT reaches its full effects before assessing whether it is adequately controlling your MS and considering another change in treatment.
Side effects and infections
As with any medication, DMTs for treating RRMS can cause a range of side effects. If you are having severe or debilitating side effects, you should reach out to your doctor to discuss changing medications.
Because DMTs suppress the immune system, most can increase the risk of infections. Some therapies increase the risk of infections such as progressive multifocal leukoencephalopathy (PML), a potentially life-threatening neurological infection caused by the John Cunningham virus (JCV).
If your medication is associated with PML, you will be regularly monitored for signs of JCV infection. If lab tests ever come back positive, you will be advised to switch to another medication that isn’t associated with this type of infection.
Lab test abnormalities
Many DMTs can cause subtle health issues, such as liver damage or low white blood cell counts. While they may not cause obvious health problems in the short term, they can eventually increase the risk of serious complications. If lab tests that monitor these problems show ongoing abnormalities, switching DMTs may be recommended.
With some therapies, the body can develop antibodies against the medication that make it less effective and increase the risk of complications. When taking these DMTs, you will be tested for antibodies as appropriate. If tests come back positive, you will usually be advised to switch treatments.
Trouble with adherence
DMTs are most effective when taken exactly as prescribed; doctors may refer to it as being adherent to the medication. This is an important aspect to consider when choosing the best MS treatment for you.
DMTs for MS include oral therapies such as oral pills, injectable therapies such as those administered under the skin, and infusion therapies administered through a slow drip into the bloodstream. Each mode of administration has its own benefits and drawbacks. For example, taking a daily pill means avoiding needles, but it requires remembering to take the medication every day. On the other hand, infusions can be time-consuming and inconvenient on the day of treatment, but they are typically needed only every few weeks or months.
There are many reasons for not fully adhering to your DMT, ranging from trouble with side effects to logistical problems to simply forgetting. If you are consistently not taking your medication as recommended, it may be worth switching to another therapy you may find easier to adhere to.
Financial issues
Many DMTs, particularly newer therapies, are expensive. Lack of insurance coverage and financial problems can sometimes make it difficult or impossible for someone to access their medication.
If finances are an issue, ask your healthcare team about financial aid resources that may be able to help. Doctors may also be able to recommend a different MS treatment that is more affordable or is covered better by your insurance.
Pregnancy
While the frequency of MS relapses tends to decrease during pregnancy, relapses are often more frequent right after pregnancy ends. However, most DMTs are not recommended for use during pregnancy or breastfeeding, either because they have safety risks or because not enough data is available to make reliable recommendations.
It’s generally recommended people with MS who are planning on becoming pregnant or are pregnant should stop taking DMTs over the course of their pregnancy. When you are no longer pregnant, adjustments to your care plan may be needed or you may resume receiving your previous treatment.
These decisions are always made on a case-by-case basis by having a collaborative conversation with your healthcare team.
Discussing MS therapy changes with your doctor
Sometimes, your doctor will initiate a conversation about switching your MS treatment — for example, if MRI scans show new lesions or if lab tests reveal persistent issues. In other situations, such as if you are experiencing bothersome side effects, you may need to advocate for yourself about wanting to switch therapies.
Whatever the case, switching DMTs is not a decision to be made lightly. You and your doctor should have detailed discussions about the potential benefits of switching medications, as well as the potential risks. These discussions should also include in-depth consideration of which treatment to switch to, taking into account factors such as how the medication works and how it is administered.
Deciding to switch or not switch medications can have a huge impact on your life, so you should always voice your desires and ask questions to make fully informed decisions.
Transitioning between therapies
The actual process of switching from one DMT to another can be very simple or quite complicated, depending on the specific situation.
With some therapies, it’s possible to simply stop taking one medication and immediately start on a new one. But other therapies are designed to have long-lasting effects and may be active in the body for months after the last dose.
To minimize the risk of complications from multiple treatments being active in the body simultaneously, some treatments require a washout period where you go without treatment for some time before starting a new therapy. The length of the washout time can vary from a few weeks to several months, depending on the specific therapies in question.
An important aspect of switching therapies is that people whose MS was well controlled while on their previous therapy may experience new disease activity during the washout period. The risk for such breakthrough activity should be discussed in depth and included in weighing the potential benefits and risks of switching treatments.
Emerging therapies and treatments
When considering a treatment switch, options aren’t always limited to approved DMTs. A variety of experimental therapies for RRMS are being tested in clinical trials, and you can ask your doctor if any of these trials might be suitable for you.
Participating in clinical research comes with potential benefits as well as possible risks. Many trials are exploring cutting-edge therapies, including some aimed at repairing myelin — the protective fatty layer around nerve fibers that is damaged in MS — which is not addressed by current DMTs.
However, these treatments are experimental, so their safety profile is not fully established, and there’s no guarantee that they will be effective. It’s also possible you are given a placebo instead of the experimental therapy depending on the trial design.
If you are interested in participating in clinical research opportunities, your healthcare team can be an invaluable resource. They can help you find suitable studies, determine which ones you may be eligible for, and discuss the potential benefits and risks of participating in specific trials.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.