MS Has 3 Distinct Subtypes, Study of MRI Brain Patterns Using AI Reports
Written by |
Using artificial intelligence (AI) on imaging data collected from multiple sclerosis (MS) patients, researchers were able to classify these people into three new disease subtypes, each distinct from the current groupings determined by symptoms.
These new subtypes may allow doctors to better determine those patients more likely to have disease progression, and which treatments might best benefit an individual, researchers said.
The study, “Identifying multiple sclerosis subtypes using unsupervised machine learning and MRI data,” was published in Nature Communications.
Historically, MS has been classified into types based on how the disease presents in the clinic, but this classification doesn’t account for the underlying cause of disease, which can make it hard to determine optimal treatment.
“Currently MS is classified broadly into progressive and relapsing groups, which are based on patient symptoms; it does not directly rely on the underlying biology of the disease, and therefore cannot assist doctors in choosing the right treatment for the right patients,” Arman Eshaghi, MD, PhD, a co-author of the new study, said in a press release.
“Here, we used artificial intelligence and asked the question: can AI find MS subtypes that follow a certain pattern on brain images?,” said Eshaghi, a senior research fellow at University College London (UCL).
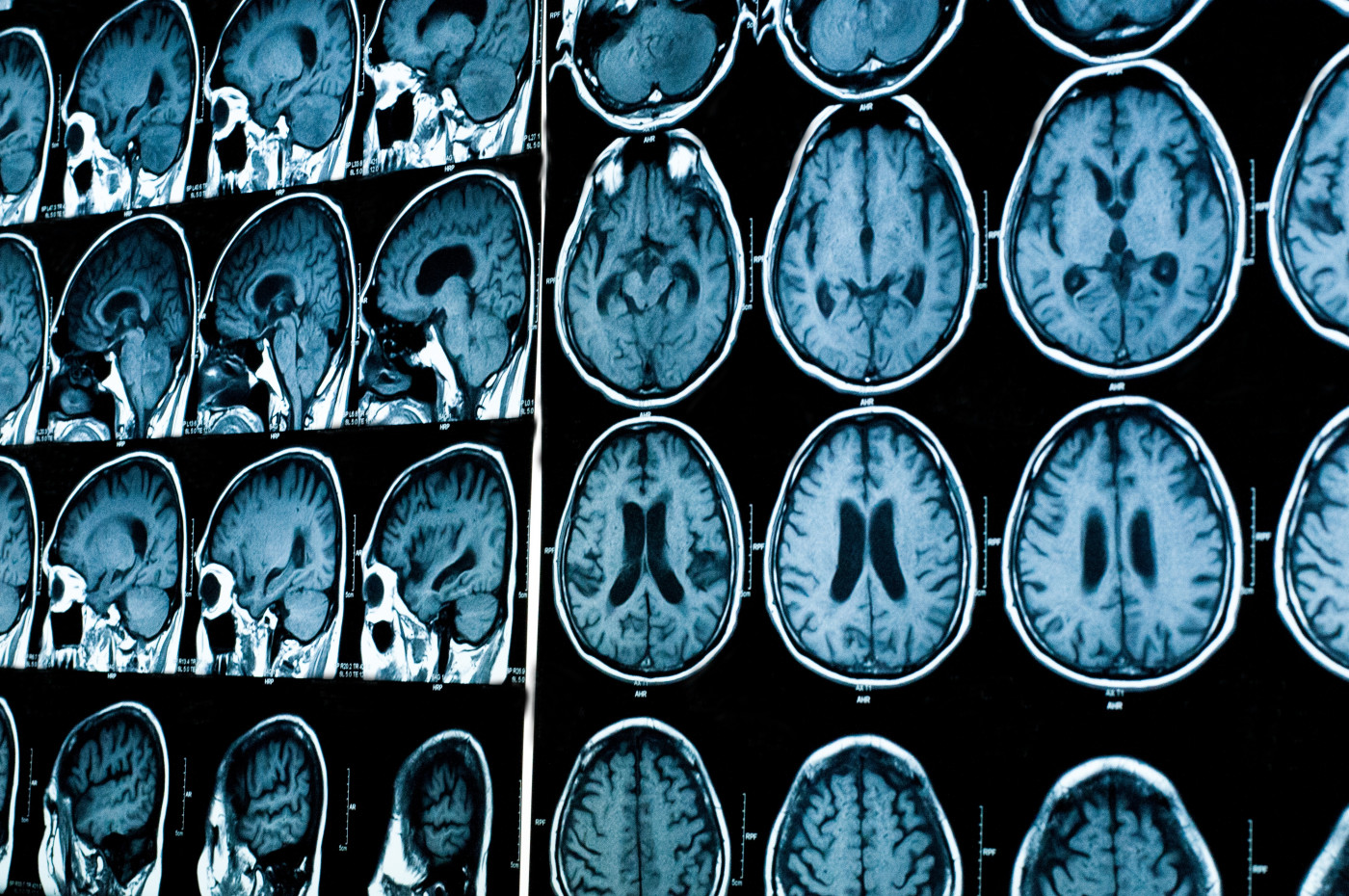
Researchers took brain imaging data, obtained via magnetic resonance imaging (MRI) scans during various clinical trials, covering 6,322 people with MS. They then fed these data into an AI program.
The program was designed to look for patterns in brain images over time, and to find statistically meaningful connections between these patterns and clinical outcomes.
AI identified three distinct MS subtypes: a “cortex-led” subtype, characterized by early tissue shrinkage (atrophy) in the outer layer of the brain; a “normal-appearing white matter-led” (NAWM) subtype, characterized by diffuse tissue irregularities in the middle of the brain; and a “lesion-led” subtype, characterized by early and extensive accumulation of areas of brain damage (lesion load), followed by severe atrophy in several brain regions.
These subtypes were further validated with data from another 3,068 MS patients, all clinically and demographically similar to first group used to train the AI. In both datasets, the cortex-led subtype was most common, and the lesion-led subtype the most aggressive — but also the subtype most likely to show treatment response among relapsing and progressive patients in clinical trials.
No differences were seen among the three subtypes in terms of patient age or sex.
Compared to those with the other two subtypes, individuals with lesion-led MS had significantly greater disability (as assessed with the Expanded Disability Status Scale, or EDSS), the longest disease duration, and more brain lesions across timepoints. Atrophy was also more extensive in these patients, who had smaller brains and less volume in other brain regions.
The lesion-led subtype also was linked with a faster rate of disability progression. Individuals with this subtype were about 30% more likely than those with the cortex-led subtype to have confirmed disability progression after 24 weeks.
Disease activity — including both relapse rates and the appearance of brain lesions — was higher in lesion-led MS than in the other subtypes. The researchers also demonstrated that the imaging-based data could be combined with other clinical data to further improve disability-related prognoses.
Notably, these MRI-based subtypes were better at predicting disability progression than the four types of MS now in wide use: clinically isolated syndrome, relapsing-remitting MS, secondary progressive MS, and primary progressive MS.
Because the researchers used clinical trial data, they were able to make preliminary estimates of treatment response among these three types. Findings indicated that trial patients with the lesion-led subtype were more responsive to treatments that included Ocrevus (ocrelizumab), Tysabri (natalizumab), and rituximab.
Lesion-led patients given the active treatment had slower disability progression than those with this subtype given a placebo or other comparator. No such difference was found among people with the other two subtypes, NAWM or cortex-led MS.
“We have identified MRI-based subtypes that provide insights into the pathobiological mechanisms of MS and predict disease activity, disability progression, and treatment response better than conventional clinical phenotypes,” the researchers concluded.
Since MRIs are part of routine care for MS patients, these subtypes could be easily integrated into use in existing clinical practice and in clinical trials testing new MS therapies, they added.
“With the help of AI and large datasets, we have made the first step towards a better understanding of the underlying disease mechanisms which may inform our current clinical classification. This is a fantastic achievement and has the potential to be a real game-changer, informing both disease evolution and selection of patients for clinical trials,” Alan Thompson, MD, study co-author and dean of the UCL faculty of brain sciences, said in a separate press release.


