What does MS spasticity feel like?
Last updated April 22, 2024, by Susie Strachan

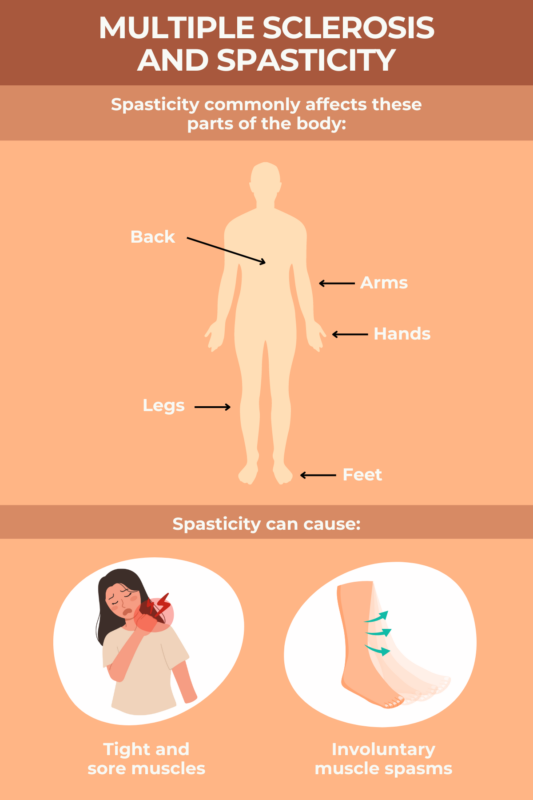
It is estimated as many as 90% of people with multiple sclerosis (MS) will experience some form of muscle stiffness or tightness — also known as spasticity.
These symptoms are often accompanied by muscle spasms or sudden, involuntary muscle movements that can make a limb kick or jerk in an uncontrolled manner.
MS spasms may cause anything from mild discomfort to significant pain and impairment in your daily life, making it difficult to walk or perform daily tasks. It also increases the risk of falls.
Treatment generally involves medications, as well as physical and occupational therapy for pain management, and using assistive devices to make living with MS spasticity easier.
What is MS spasticity?
Spasticity develops because your muscles become tight over time, which can make it hard to move. It can also cause muscle stiffness, a feeling of heaviness, and pain.
MS is a disease that occurs when the immune system attacks the central nervous system (the brain and spinal cord). Such attacks cause damage to the myelin sheath — the protective covering of nerve fibers — and disrupt communication between the nerves and muscles. This disruption can lead to abnormal nerve signals and overactivity of muscles.
How does spasticity affect the body?
Spasticity and its spasms can affect any part of the body, but it is more common for people with MS to be affected in their legs, groin, and buttocks.
You may experience increased muscle tightness or stiffness that makes it difficult to relax muscles fully. This stiffness can cause you to have difficulty moving and affect your posture and range of motion.
Symptoms of MS spasticity vary from person to person in intensity. They also may change over time in the same person, including throughout the day.
Spasticity in MS can make it difficult to walk or perform other daily tasks. Having weak muscles, which is common in MS, also can worsen spasticity symptoms and affect your balance, increasing the risk of falls.
When muscles affected by spasticity remain in a shortened position for prolonged periods, they are more prone to developing joint contractures. These are abnormal shortening or tightening of muscles, tendons, or ligaments around a joint. Contractures can impair joint mobility and function, and people may require intervention to prevent further complications.
Triggers
MS spasticity triggers include:
- very hot or cold temperatures
- humidity
- infections
- sudden movements
- wearing tight clothing.
Extreme temperatures, particularly heat, can worsen spasticity. Heat sensitivity is a common symptom of MS. Exposure to hot weather, saunas, hot baths, or overheated environments can trigger spasticity.
Spasticity also can be triggered by strenuous exercise or prolonged periods of standing or walking.
Fatigue also can trigger spasticity. Fatigue in MS can be a direct result of myelin damage and nerve signaling problems. This type of fatigue is often different from what people who don’t have MS may experience: It is sudden, more severe, aggravated by heat or humidity, and not affected by restful sleep.
Infections, such as urinary tract infections or respiratory infections, may also trigger spasticity, because illnesses and infections can lead to systemic inflammation in the body. People with infections are more likely to experience fever, dehydration, and fatigue, all of which can contribute to spasticity.
Wearing tight or restrictive clothing can increase muscle stiffness and spasticity by increasing pressure on your muscles and restricting blood flow, as well as limiting range of motion, and increasing heat retention.
Emotional stress or anxiety can trigger a physiological response, including increased muscle tension and heightened nerve activity, which can lead to spasticity.
What does MS spasticity feel like?
Feelings of MS spasticity can range from mild twitching to more intense and painful involuntary muscle spasms. The pain may be localized to a specific muscle group radiating out to adjacent areas.
Along with involuntary jerking movements, spasticity can make it challenging to fully relax the affected muscles, leaving them stiff and sore. It can sometimes feel as though the muscles have become locked in a position.
Former Multiple Sclerosis News Today columnist Ed Tobias, who has MS, wrote about how he had to find the right treatment to help control the cramping and tightness of his leg muscles and the resulting pain.
In consultation with his doctor, Tobias switched medications multiple times to better control spasticity in “both my jerky legs at bedtime and the sharp pains that occasionally traveled down my legs from my hips to my knees.”
Do symptoms get worse in the night?
For some people with MS, spasticity symptoms can become worse at night, causing you to wake up and lose sleep.
Benjamin Hofmeister, a Multiple Sclerosis News Today columnist who was diagnosed with MS in 2014, described how MS-induced spasticity would wake him up multiple times during the night.
“Whenever that happened, it was next to impossible to fall back asleep,” he wrote.
There are a number of reasons why spasticity symptoms can get worse at night:
- As you sleep, you typically spend several hours in a relatively stationary position. Lack of movement can contribute to muscle stiffness and tightening.
- Changing your position in bed, such as rolling over, can trigger muscle spasms that may be painful and also wake you up.
- If the medications you’re taking for spasticity wear off during the night, you may also experience spasticity.
Treatment options
The goal of treatment for MS spasticity is to reduce muscle stiffness, spasms, and discomfort while improving mobility.
It’s important to work with healthcare professionals to develop a personalized treatment plan. It may include a combination of medications, physical and occupational therapy, along with complementary therapies such as massage and acupuncture.
There are medications to help manage MS-related spasticity. These generally work by tamping down the signals from nerve cells that tell muscles to contract, which reduces muscle contractions. Cannabis-based products also may ease spasticity symptoms.
A physical therapist can show you stretching and range-of-motion exercises to help improve flexibility, reduce muscle stiffness, and lessen the severity of spasticity symptoms.
An occupational therapist can recommend assistive devices — such as braces, splints, and mobility aids — and adaptive equipment, such as reachers or utensils with large handles, to maintain your mobility and help you perform daily tasks more easily.
They can make suggestions for home and workplace modifications, including handrails, grab bars, and ramps, to improve accessibility and safety.
Complementary therapies such as massage and acupuncture may help relax muscles and reduce muscle tension.
Self-management strategies
In addition to medical treatments and therapies, lifestyle changes may help you manage muscle spasticity and MS.
The following self-care strategies for spasticity may help:
- Try exercises such as stretching, aerobic activities, and strength training to help improve flexibility, mobility, and muscle strength while reducing muscle stiffness and spasms.
- Manage your energy levels by pacing your activities, incorporating rest breaks, and avoiding overexertion to prevent triggering or worsening spasticity.
- Identify and avoid potential triggers, such as extreme temperatures, fatigue, and stressful situations, to help prevent symptom flare-ups.
- Wear loose-fitting and comfortable clothing to minimize the risk of triggering or worsening spasticity symptoms.
- Practice relaxation techniques such as meditation or deep breathing to reduce stress and improve mental health.
- Establish a regular sleep schedule, create a relaxing bedtime routine, and set up a good sleep environment in a dark and quiet room.
- Eat a balanced and nutritious diet to support overall health and potentially help with MS symptom management, including spasticity.
Always discuss any lifestyle modifications you are considering with your personal healthcare providers first to ensure these are safe and appropriate for your condition.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.