Rebif Cost-effective and Can Reduce Brain Lesions in RRMS Patients, Data Show
Written by |
Merck KGaA presented new evidence supporting the safety and clinical efficacy of Rebif (interferon beta-1a) for relapsing-remitting multiple sclerosis (RRMS) at the 5th Congress of the European Academy of Neurology (EAN), June 29–July 2 in Oslo, Norway.
The company, known as EMD Serono in the U.S. and Canada, presented 16 studies that included new clinical safety and efficacy data on Rebif, as well as Mavenclad (cladribine tablets), and the investigational therapy evobrutinib.
Rebif decreases the frequency of relapse and delays the onset of some of the physical incapacity associated with MS.
At EAN 2019, in a presentation titled, “Subcutaneous Interferon β-1a: 10 years of the UK Multiple Sclerosis Risk Sharing Scheme,” data from the U.K. MS Risk-sharing scheme, set up in 2002 by that nation’s department of health, was presented. Researchers used the data to assess the cost-effectiveness of various disease-modifying treatments for MS, including Rebif, over 10 years.
In all, 1,635 MS patients treated with Rebif were analyzed. Throughout the 10-year period, Rebif was considered to be cost-effective.
Disease progression was monitored every two years using the Expanded Disability Status Scale (EDSS), which ranges from zero to 10 — higher numbers represent a greater degree of disability. Results showed that treatment with Rebif decreased EDSS scores.
The data therefore represent ‘real-world’ evidence of the long-term benefits of Rebif.
In another presentation titled, “Rapid reduction of lesion accumulation in specific white matter tracts as assessed by lesion mapping in RRMS patients treated with IFN beta-1a,” researchers presented data from the randomized, multi-center Phase 3 IMPROVE study (NCT00441103) evaluating the effects of Rebif compared to placebo in patients with RRMS.
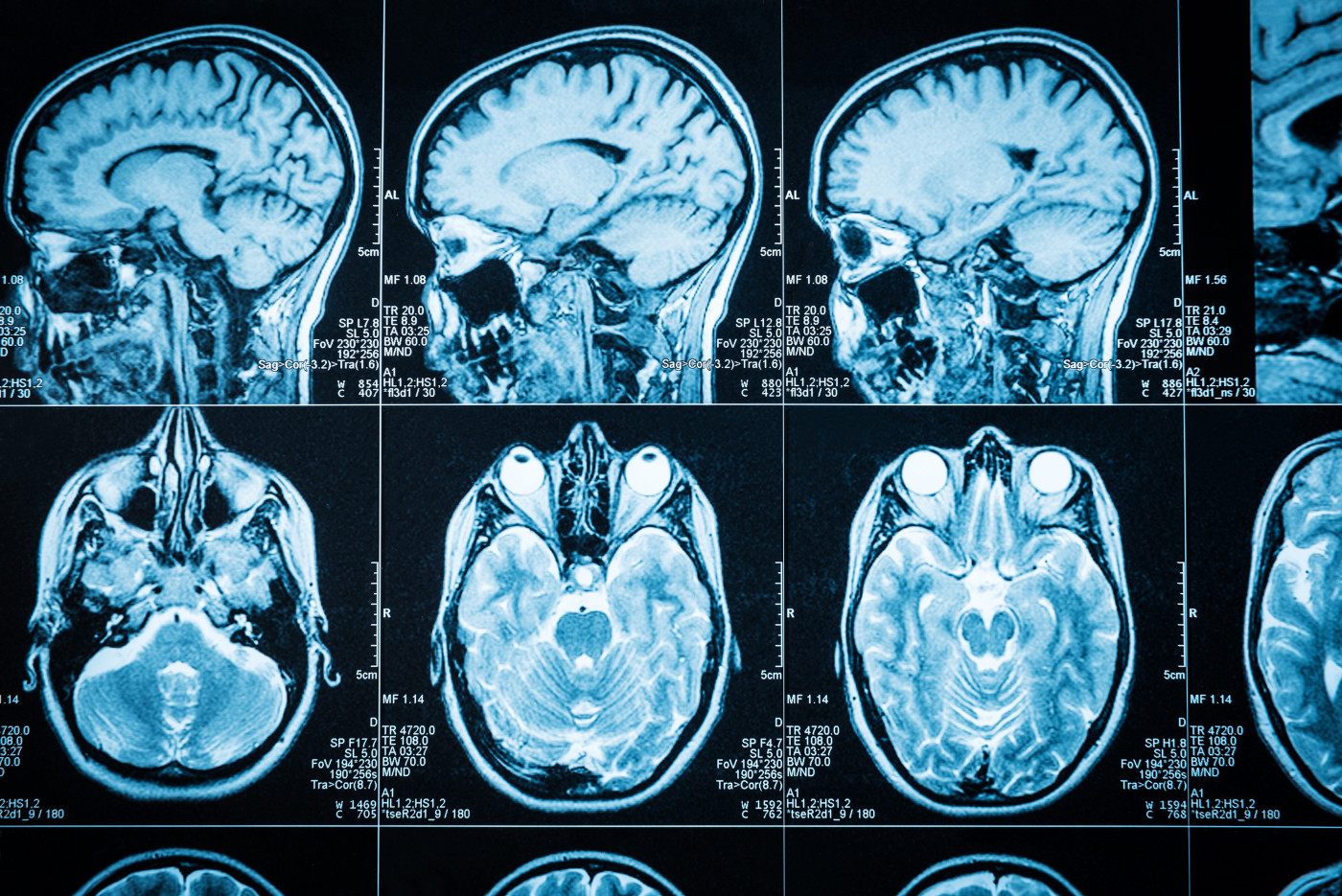
In the IMPROVE study, patients were given 44 micrograms of Rebif three times a week, and underwent magnetic resonance imaging (MRI) scans every four weeks.
Post-hoc analysis showed that the number of combined unique active lesions decreased by 50% in patients treated with Rebif compared to placebo. Mapping of lesions showed that Rebif reduced by 50% or more the lesions in specific brain regions associated with clinical manifestations of MS compared to placebo. The decrease in frequency of these lesions by Rebif started at week four of treatment.
In a third presentation about Rebif data, titled “Dynamics of pseudo-atrophy in RRMS patients treated with interferon beta-1a as assessed by monthly brain MRI,” researchers presented results from a post-hoc analysis of MRI data from the IMPROVE study. Changes in brain volume loss in two different types of tissue, known as grey and white matter, were analyzed.
Brain volume loss and brain lesion atrophy correlate with the physical disability associated with MS. Measuring changes in brain volume loss can then be used to assess the efficacy of treatments; however, this is tricky for anti-inflammatory therapies such as Rebif, in which accelerated brain volume loss is seen after initiating treatment — a phenomenon called pseudo-atrophy.
Results showed that in up to 16 weeks of treatment, the decrease in grey matter volume in RRMS patients was significantly greater with Rebif compared with the placebo (0.27% vs 0.14% per month, respectively). For white matter, treatment with placebo decreased the volume by 0.067% per month, compared to 0.116% for Rebif, although this difference was not significant.
“Monthly acquired MRI from IFN beta-1a-treated patients showed more pronounced pseudo-atrophy effect in grey than white matter, with maximum decrease up to week 20,” the researchers stated.
Analysis of the MRI data for longer periods of time (over 40 weeks) indicated that the decrease in both white and grey matter appeared to be maximum up to 20 weeks, after which it reached a plateau.
“The wealth of new data [presented] at EAN 2019, from both our approved medicines and our pipeline in MS, highlight our commitment to making further advances for people living with this chronic disease,” Luciano Rossetti, the head of global research & development for the biopharma business of Merck KGaA, said in a press release.


