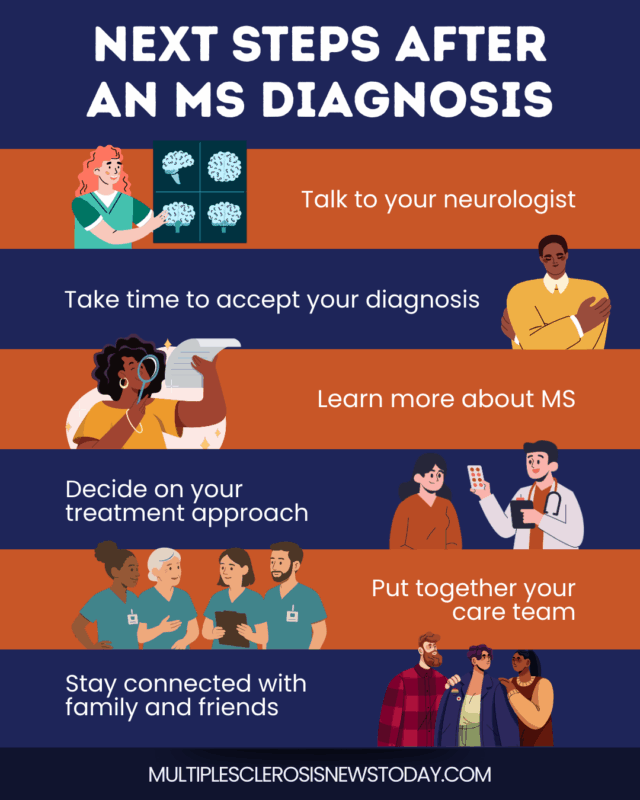
FAQs about after an MS diagnosis
Support starts with your healthcare team, who provide and modify treatment for multiple sclerosis (MS) and its symptoms. They may be able to connect you to community resources for peer counseling, mental health counseling, and financial support. They may also tell you about the latest in MS news and research.International MS charities and organizations offer online and in-person support groups. Many of them have MS navigators who can answer your questions.
There are reasons you may want a second opinion. Multiple sclerosis (MS) can be mistaken for a number of other chronic and debilitating diseases that affect the central nervous system, which a neurologist must rule out before making a diagnosis. Also, there isn’t one specific test for MS. Instead, neurologists rely on clinical assessment tests such as magnetic resonance imaging (MRI), spinal tap, vision tests, and an evoked potential test. For peace of mind, you can always ask for a second opinion. Find a medical professional who is not connected to the first team of healthcare specialists who made the initial diagnosis.
Multiple sclerosis (MS) treatment falls into three categories: disease-modifying therapies, relapse management therapies, and those treating symptoms. Disease-modifying therapies are medications that can change the course of the disease. Relapse management medications treat MS flare-ups and promote recovery. MS symptom treatment is aimed at controlling common MS symptoms, such as fatigue, chronic pain, muscle stiffness and involuntary spasms (spasticity), the ability to walk and move, bladder and bowel problems, sexual dysfunction, and mental health.
You can get health insurance for multiple sclerosis (MS) treatment and care in the U.S. at the federal and state levels by buying it through private or workplace insurance plans, or through the Department of Veterans Affairs.
Maintaining your physical health after a diagnosis of multiple sclerosis (MS) may mean changing your diet by eating more nutritious foods and doing gentle exercises. It also helps to stop smoking tobacco and drinking alcohol, as both can worsen MS symptoms. MS can also affect the part of the brain that controls emotions, so you may want to consider psychological counseling. MS support groups, and connecting with family and friends is another way to boost your mental health.
 Fact-checked by
Fact-checked by