MS and chronic pain: Treatment and management
Last updated May 14, 2025, by Susie Strachan

Chronic pain is common in multiple sclerosis (MS), affecting between 50% and 75% of people at some point during the course of their disease.
Living with chronic pain from MS can feel different from person to person. It might feel like burning, stabbing, or tingling sensations, or can a deep, aching pain. This type of pain lasts for a long time, from more than three months to several years, and can happen daily.
Different body parts may be affected, with MS-related pain occurring in the upper and lower back, shoulders, pelvic region, jaw and teeth, and even the back of your head and ears. You might also experience tightness or squeezing, like the so-called MS hug sensation, around your chest or torso.
Fortunately, there are strategies and treatments available to help reduce chronic pain. These include medications, complementary treatments such as physical therapy, and lifestyle changes that can help your mood, reduce fatigue, and make it easier to manage pain from MS.
How chronic pain affects people with MS
In MS, your immune system attacks your brain and spinal cord, damaging the protective covering of nerves and causing nerve cell loss.
This damage can disrupt normal nerve function, causing abnormal nerve signals that lead to pain and other symptoms affecting your muscles, coordination, speech, and more.
Pain can also affect your sleep, mental health, relationships, and finances.
For example, pain-related sleep disturbances can worsen fatigue and mood issues, creating a cycle of pain and emotional distress. Anxiety and depression can heighten pain perception, making it feel more intense.
The cognitive impacts of persistent pain, such as trouble concentrating, can also affect how you function on a day-to-day basis in both your personal and professional life.
Finally, living with chronic pain can be expensive due to ongoing healthcare costs and lost income if your pain makes it harder to work.
Common types of pain in MS
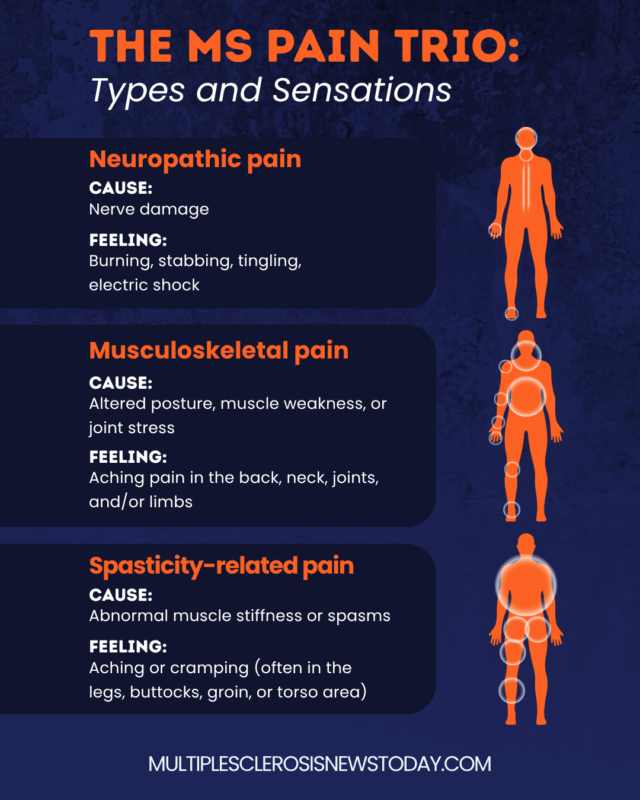
Pain in MS can be complex, with various types overlapping or contributing to one another. The more common types include neuropathic pain, musculoskeletal pain, and spasticity-related pain — pain related to abnormal muscle spasms and tightness.
Neuropathic pain
Neuropathic pain in MS is caused by nerve damage, leading to sensations like burning, tingling, or electric shocks. Neuropathic pain can include:
- dysesthesia, such as burning, stabbing, itching, or aching sensations, commonly affecting the legs, arms, face, or chest
- a sudden electric shock-like sensation called Lhermitte’s sign that runs down the spine, may radiate into the limbs, and is usually triggered when the neck is bent forward
- an intense and sudden pain called trigeminal neuralgia that typically affects one side of the face, including your jaw.
There is evidence that women with MS, as well as those who have lived with the disease for longer or have a higher level of disability, may be more likely to experience neuropathic pain.
Musculoskeletal pain
Musculoskeletal pain results from muscle strain, joint stress, or altered posture due to muscle weakness or spasticity. This type of pain can include joint pain, neck and back pain, and leg and arm pain.
Lower back pain may also occur. This pain typically stems from changes in mobility and muscle weakness.
Spasticity-related pain
Spasticity-related pain involves muscle stiffness or spasms that cause aching or cramping. Spasticity can make it difficult to relax your muscles fully and is more commonly found in the legs, groin, and buttocks.
In some individuals, this symptom worsens during the night, and the spasms and pain can disrupt sleep. There are also other types of pain associated with MS:
- Secondary pain may develop from immobility or compensating for weakness, leading to overuse of unaffected muscles, such as in your hands, feet, hips, or knees.
- Optic neuritis is pain behind the eyes caused by optic nerve inflammation.
- Headaches can be more common in MS due to neuroinflammation, nerve damage, and the side effects of MS medications, as well as other MS-related conditions like spasticity or sleep disturbances.
- MS hug pain describes a feeling of tightness, pressure, or a hug around the chest or abdominal area, which is caused by nerve damage or muscle spasms affecting the muscles between the ribs.
MS pain treatment options
When deciding on the proper treatment specific to you, your MS healthcare team will consider factors such as the severity and type of your pain, as well as your preferences and any other health conditions you may have.
They may recommend certain medications to help manage your pain, including:
- anticonvulsants, which can help manage neuropathic pain by stabilizing nerve activity
- antidepressants, shown to alleviate neuropathic pain
- analgesics, or painkillers, to help with musculoskeletal pain
- muscle relaxants, which help ease spasticity and the associated pain
- corticosteroids if your pain arises or worsens during a relapse, though these are not usually considered as a primary MS treatment for chronic pain.
Other medications have been explored for treating MS pain, such as botulinum toxin and opioid analgesics. However, research indicates these treatments have limited effectiveness and may have concerning side effects.
Alternative and emerging treatments
Some studies suggest cannabis may help with MS-related pain, but the findings are mixed, so it’s important to discuss the risks and benefits of using cannabis for MS pain symptoms with your healthcare provider.
Emerging treatments, such as noninvasive stimulation techniques, are also being studied to see if they can help manage MS-related pain. These treatments may reduce the sensation of pain by blocking pain signals or encouraging the release of natural pain-relieving chemicals.
Complementary pain management strategies
In addition to medications, other therapeutic approaches may help with MS pain management, such as physical and occupational therapy, psychological therapies, and other complementary treatments.
Physical and occupational therapy
Physical and occupational therapy can help with pain relief by improving your movement, mobility, and posture.
These therapies can also teach you strategies to reduce strain on your body, and how to find ways to carry out daily activities more comfortably.
Psychological approaches
Psychological approaches such as cognitive behavioral therapy (CBT), mindfulness, and meditation can help with the mental and emotional aspects of living with chronic pain.
These techniques can teach you how to manage stress, cope with pain, and change negative thought patterns that may contribute to how you experience pain.
Other complementary treatments
Other complementary treatments, such as body massages, hydrotherapy, and acupuncture, may provide relief for some people. These therapies aim to relax muscles, improve circulation, and promote healing.
Talk with your healthcare provider to determine which strategies best suit your needs.
Lifestyle changes that may reduce pain
Adopting healthy lifestyle practices like regular exercise, stress reduction, social activity, and more may help reduce your MS-related pain.
- Engaging in light activity, like walking or swimming, or structured fitness routines, can help strengthen muscles, reduce stiffness, improve flexibility, boost circulation, and support mobility, making it easier to manage pain in the long term.
- Reducing stress through deep breathing, mindfulness, and meditation may make it easier to manage your pain by calming the mind and body.
- Connecting with friends, family, or MS support groups, and engaging in activities you enjoy can help improve your mental health.
- Developing a calm bedtime routine, creating a comfortable sleep environment, and maintaining consistency can contribute to good quality sleep, which in turn helps your body repair itself and reduces the impact of fatigue.
- Eating a well-balanced diet that includes nutrient-rich foods such as fruits, vegetables, whole grains, and healthy fats can support your body’s ability to manage pain and promote healing.
- Staying hydrated can help you maintain your energy levels.
Living with chronic pain from MS can be overwhelming, but with the right combination of treatments, lifestyle adjustments, and support, it’s possible to find relief and improve your quality of life.
Every person’s experience with MS is unique. Work with your healthcare team to determine which treatments and therapies are right for you.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.