Mouse Study Links Cortical Inflammation to Immune Cell Destruction
Written by |
Multiple sclerosis (MS)-associated inflammation in the cerebral cortex — the outermost layer of the brain that is involved in cognitive function — prompts the destruction of neural connections by specific immune cells, according to a study in a mouse model of MS.
These immune cells targeted dendritic spines (nerve cell communication structures) containing abnormally high levels of calcium — a dysregulation previously associated with nerve fiber degeneration in MS.
Importantly, blocking the activation of these immune cells, called phagocytes, successfully prevented the loss of cerebral cortex synapses (sites of neural communication) in the mice, highlighting that similar approaches may help prevent disease progression in people with MS.
“Targeted inhibition of specific types of immune cells can slow synapse damage down, and offers an interesting new therapeutic approach,” Martin Kerschensteiner, MD, one of the study’s co-senior authors, said in a press release. Kerschensteiner is the director of the Institute for Clinical Neuroimmunology at Ludwig-Maximilians University Munich, in Germany.
The study, “Phagocyte-mediated synapse removal in cortical neuroinflammation is promoted by local calcium accumulation,” was published in the journal Nature Neuroscience.
MS is an inflammatory disease characterized by abnormal immune attacks against the protective sheath around nerve cell fibers, which comprise the white matter of the brain. However, as the disease progresses, the gray matter of the brain — made up of nerve cell bodies, axon terminals, and dendrites — also becomes damaged.
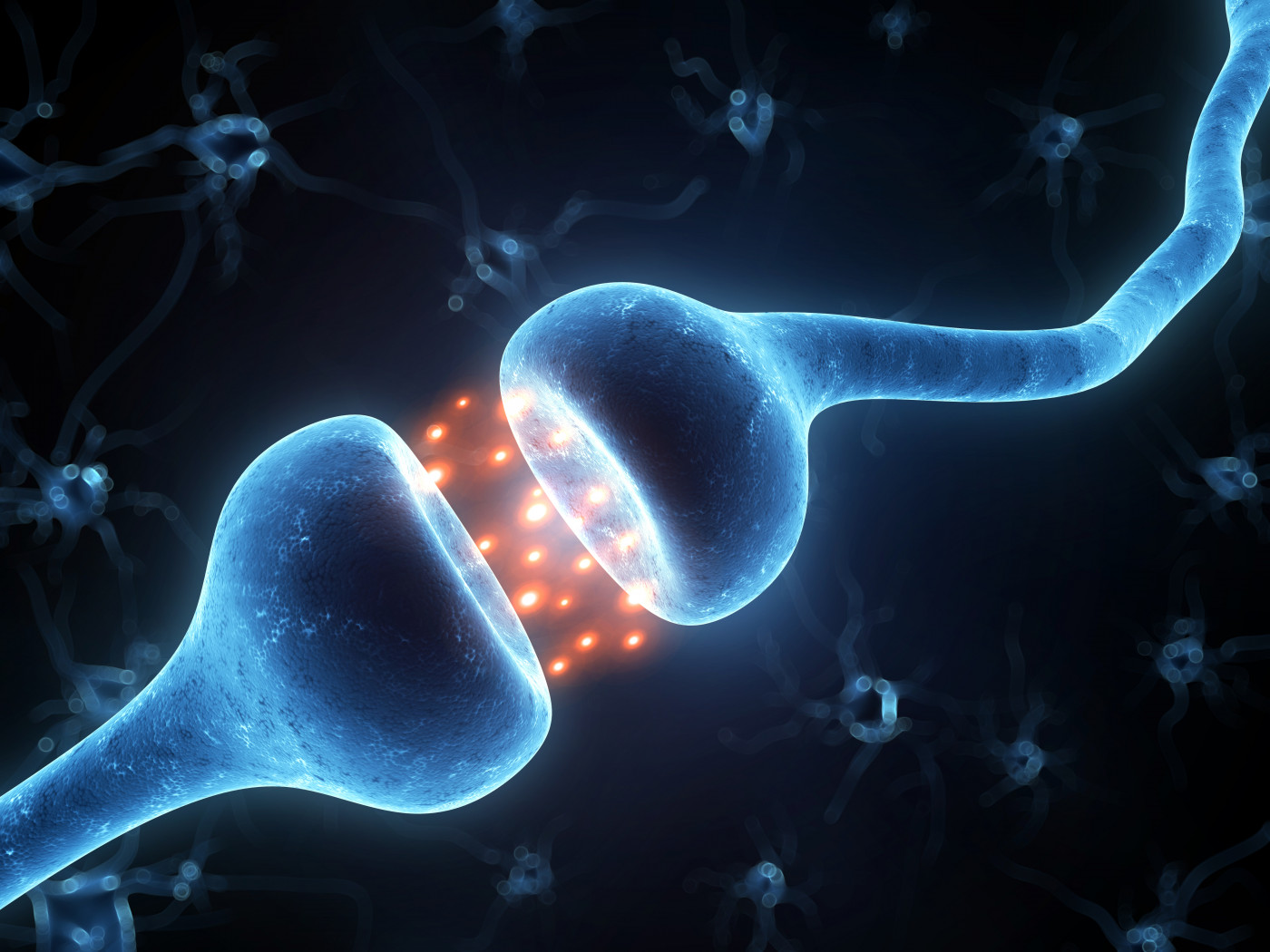
Axon terminals are the tips of long nerve cell fibers, while dendrites are shorter fibers containing numerous branches called dendritic spines. The site of near contact between these structures, called a synapse, is where nerve cells transmit chemical and electrical signals to one another.
Notably, loss of synapses is an early indicator of damage to the cerebral cortex (the outermost gray matter area) in cases of progressive MS, and lesions in this region have been associated with cognitive difficulties in MS patients.
However, “how such gray matter inflammation affects neuronal structure and function is not well understood,” the researchers wrote.
Using a mouse model of MS, Kerschensteiner’s team, along with colleagues from other universities, showed that cerebral cortex inflammation reduces nerve cell activity due to a widespread loss of dendritic spines.
Further analysis showed that these structures, which are mainly associated with activating synapses, were destroyed by phagocytes — a group of immune cells that clear the body from harmful invaders, such as bacteria, and damaged or death cells by engulfing (eating) them.
“The nerve cells are effectively silenced,” said Kerschensteiner.
Phagocytes preferentially targeted dendritic spines with abnormally high levels of calcium, a molecule that plays a key role in many nerve cell functions and is therefore tightly regulated.
“We assume that the inflammation reaction itself triggers an influx of calcium, which destabilizes the spines,” said Kerschensteiner.
Thomas Misgeld, MD, a co-senior author of the study at the Technical University of Munich, said these calcium changes “in late-stage MS are reminiscent of those that can also be observed during the early phases of neurodegeneration.”
“However, much to our surprise, we discovered that this process is reversible in our model,” Kerschensteiner added. The model is based on the induction of an acute inflammatory reaction, which is resolved in a few days.
The data showed that as soon as the inflammation was resolved, the number of dendritic spines and synapses was restored, and nerve cell activity normalized. These findings contrast with the permanent cerebral cortex damage observed in people with progressive MS, the researchers noted.
“Presumably, the mechanisms responsible for recovery cannot come into effect in these patients, because the inflammation is chronic and remains unresolved,” said Doron Merkler, MD, of the University of Geneva and the study’s third co-senior author.
Moreover, treating mice with a pharmacological suppressor of phagocyte activation prevented synapse loss in the cerebral cortex, highlighting that approaches targeting phagocytes and their activity may help preserve nerve cell communication and slow disease progression.
However, such approaches must not entirely block the activity of these cells, the team noted, as they are essential for normal immune responses and toxic debris clearance.
“Overall, our study identifies synapse loss as a key [disease-associated] feature of inflammatory gray matter lesions that is amenable to immunomodulatory therapy,” the researchers wrote.


