Treatment of secondary progressive MS
Last updated Oct. 20, 2025, by Lindsey Shapiro, MS

Secondary progressive multiple sclerosis (SPMS) treatment typically requires a multidisciplinary approach that combines disease-modifying therapies (DMTs) to slow disease progression with supportive interventions to manage symptoms and maintain quality of life in SPMS.
Most people with multiple sclerosis (MS) are first diagnosed with relapsing-remitting MS (RRMS), a form of the disease marked by episodes of new or worsening symptoms (relapses) followed by periods of partial or complete recovery (remission).
Over time, many people with RRMS transition to SPMS, a form of MS in which symptoms gradually worsen, even without relapses.
As patients progress to SPMS, treatment goals and strategies often shift. The focus moves from primarily preventing relapses to slowing ongoing neurological damage, managing increasingly burdensome symptoms, and preserving independence. Still, several DMTs approved for RRMS can also be used in the SPMS stage.
SPMS treatments
SPMS treatment options depend largely on whether the disease is considered active or nonactive.
In active SPMS, people continue to experience occasional relapses and/or develop new active lesions on MRI scans, indicating ongoing inflammatory activity. By contrast, nonactive SPMS is marked by the absence of new relapses or MRI activity, and disease progression is believed to result mainly from chronic, smoldering inflammation within the brain and spinal cord that drives gradual neurodegeneration.
Active SPMS
Most DMTs approved in the U.S. are indicated for relapsing forms of MS, namely, clinically isolated syndrome, RRMS, and active SPMS. These therapies work primarily by targeting immune cells outside the brain and spinal cord to reduce the acute inflammation that causes relapses and drives the formation of new lesions.
While not all DMTs for SPMS have demonstrated a clear impact on long-term disability progression in clinical trials, treatment guidelines recommend their use in SPMS patients who still show inflammatory activity.
Typically, anyone benefiting from a DMT during the RRMS phase may continue receiving it after transitioning to active SPMS. However, if the disease later becomes nonactive, a doctor may recommend discontinuing treatment.
Injectable DMTs for active SPMS include:
- interferon-based therapies, such as Avonex, Betaseron, Extavia, Plegridy, and Rebif
- CD20 inhibitors, among them Kesimpta (ofatumumab) and Ocrevus Zunovo (ocrelizumab and hyaluronidase-ocsq)
- Copaxone (glatiramer acetate injection)
Oral DMTs for active SPMS include:
- Aubagio (teriflunomide)
- fumarate therapies such as Bafiertam (monomethyl fumarate), Tecfidera (dimethyl fumarate), and Vumerity (diroximel fumarate)
- S1P modulators such as Gilenya (fingolimod), Mayzent (siponimod), Ponvory (ponesimod), and Zeposia (ozanimod)
- Mavenclad (cladribine)
DMTs given by infusion for active SPMS include:
- anti-CD20 antibodies, such as Briumvi (ublituximab-xiiy) and Ocrevus (ocrelizumab)
- Lemtrada (alemtuzumab)
- Mitoxantrone
- Tysabri (natalizumab)
Because people with active SPMS can sometimes experience relapses, they may also need additional treatments such as glucocorticoids to manage symptoms during severe flares.
Nonactive SPMS
Nonactive SPMS is more challenging to treat because most DMTs primarily act outside the brain and spinal cord to dampen inflammation, while the mechanisms driving disease progression in nonactive SPMS are thought to occur within the brain and spinal cord.
Mitoxantrone is technically approved in the U.S. for the treatment of active and nonactive SPMS. However, due to its significant risks, including potential heart damage and an increased risk of leukemia, it is now rarely used in clinical practice.
With a lack of approved DMTs, nonactive SPMS treatment focuses mainly on symptom management, rehabilitation, and supportive care to preserve physical and cognitive function and maintain quality of life.
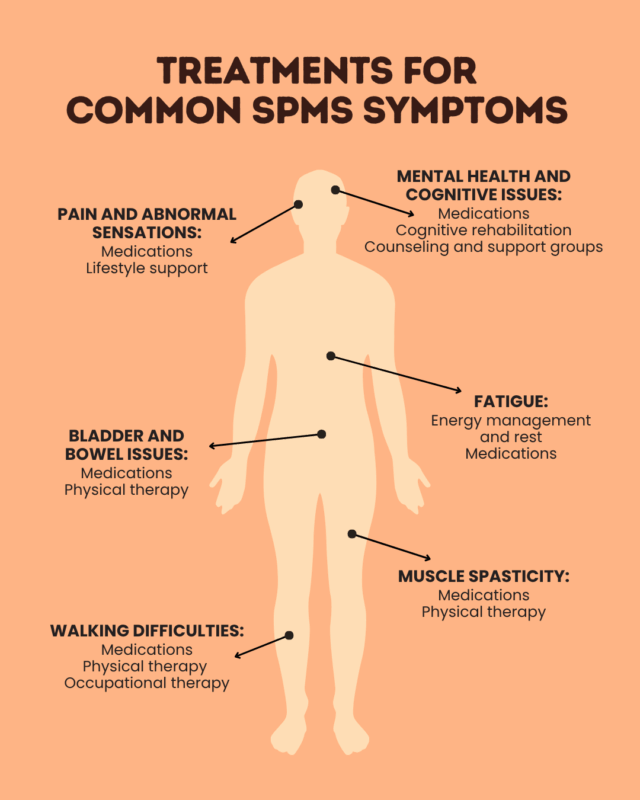
Symptom management approaches
A wide range of medications and interventions are used for managing symptoms of SPMS. These supportive treatments don’t slow disease progression, but they can make daily living with MS easier.
- Spasticity may be treated with oral muscle relaxants or injections of botulinum toxin products.
- Fatigue management in MS largely relies on lifestyle changes, but off-label medications may sometimes be used.
- Walking difficulties may be treated with Ampyra (dalfampridine) or the Portable Neuromodulation Stimulator (PoNS) device.
- Bladder and bowel problems can be managed with lifestyle changes and various medications.
- Nerve pain or abnormal sensations are treated with off-label use of antiseizure medications or antidepressants.
- Mental health and emotional issues can be treated with antidepressant and antianxiety medications, while pseudobulbar affect — sudden bursts of uncontrollable laughter or crying — can be treated with Nuedexta (dextromethorphan and quinidine).
Beyond SPMS medications, several nondrug treatments for SPMS may be used to control symptoms and maintain independence.
- Physical therapy for MS uses tailored exercises to reduce spasticity and improve mobility. It can also help strengthen the pelvic floor muscles to ease bladder issues.
- Occupational therapy for MS teaches patients strategies to adapt to mobility or cognitive limitations, and supports independent living.
- Counseling and cognitive rehabilitation in MS can help patients manage the cognitive and emotional challenges associated with the disease.
Because a person’s specific needs will likely change as SPMS progresses, symptom management in SPMS relies on ongoing communication with a multidisciplinary care team.
Lifestyle and supportive care
Supportive care for MS patients often involves lifestyle changes that can help ease symptoms and reduce the daily impact of SPMS. These may include:
- getting regular exercise
- eating a healthy and well-balanced diet
- managing stress and getting enough sleep
- building a support network and finding coping strategies to manage mental health and MS more effectively
- using mobility aids or making home modifications to make daily activities safer and easier
People with SPMS should avoid making major lifestyle changes without first consulting their care team, who can help identify approaches that are safe and effective, and help integrate them into a person’s overall treatment plan.
Clinical trials and emerging treatments
Various experimental treatments are being tested in SPMS clinical trials, which focus particularly on the chronic inflammation and neurodegeneration within the brain and spinal cord that drive SPMS disability progression.
Promising areas of investigation include:
- Bruton’s tyrosine kinase inhibitors and others therapies that target brain-resident immune cells involved in SPMS progression
- remyelinating treatments, designed to restore myelin, the protective coating around nerve fibers that’s progressively lost in MS
- neuroprotective treatments, which help protect nerve cells from further damage
- CAR T-cell therapies, which seek to reprogram the immune system to stop attacking healthy tissues
If eventually approved, some of these emerging treatments for SPMS could provide new options for slowing progression in SPMS.
People who wish to participate in clinical trials should ask their care team about available opportunities and whether any ongoing trials might be appropriate for them.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.